Deposition Date
2025-07-04
Release Date
2025-07-16
Last Version Date
2025-11-26
Entry Detail
PDB ID:
9PFI
Keywords:
Title:
Crystal structure of SARS-CoV-2 Mpro Mutant P132H
Biological Source:
Source Organism(s):
Expression System(s):
Method Details:
Experimental Method:
Resolution:
1.81 Å
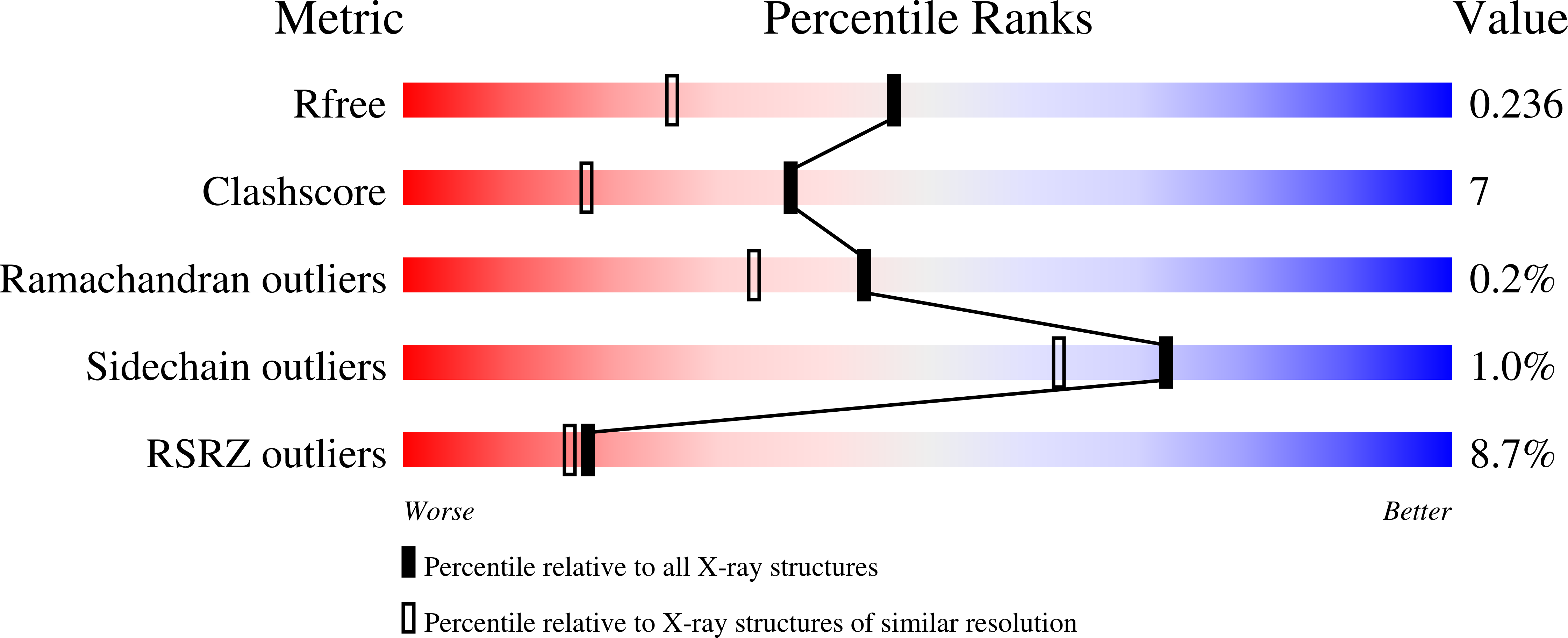
R-Value Free:
0.23
R-Value Work:
0.18
R-Value Observed:
0.19
Space Group:
P 21 21 21