Deposition Date
2024-03-13
Release Date
2025-02-12
Last Version Date
2025-04-02
Entry Detail
Biological Source:
Source Organism(s):
Homo sapiens (Taxon ID: 9606)
Expression System(s):
Method Details:
Experimental Method:
Resolution:
2.30 Å
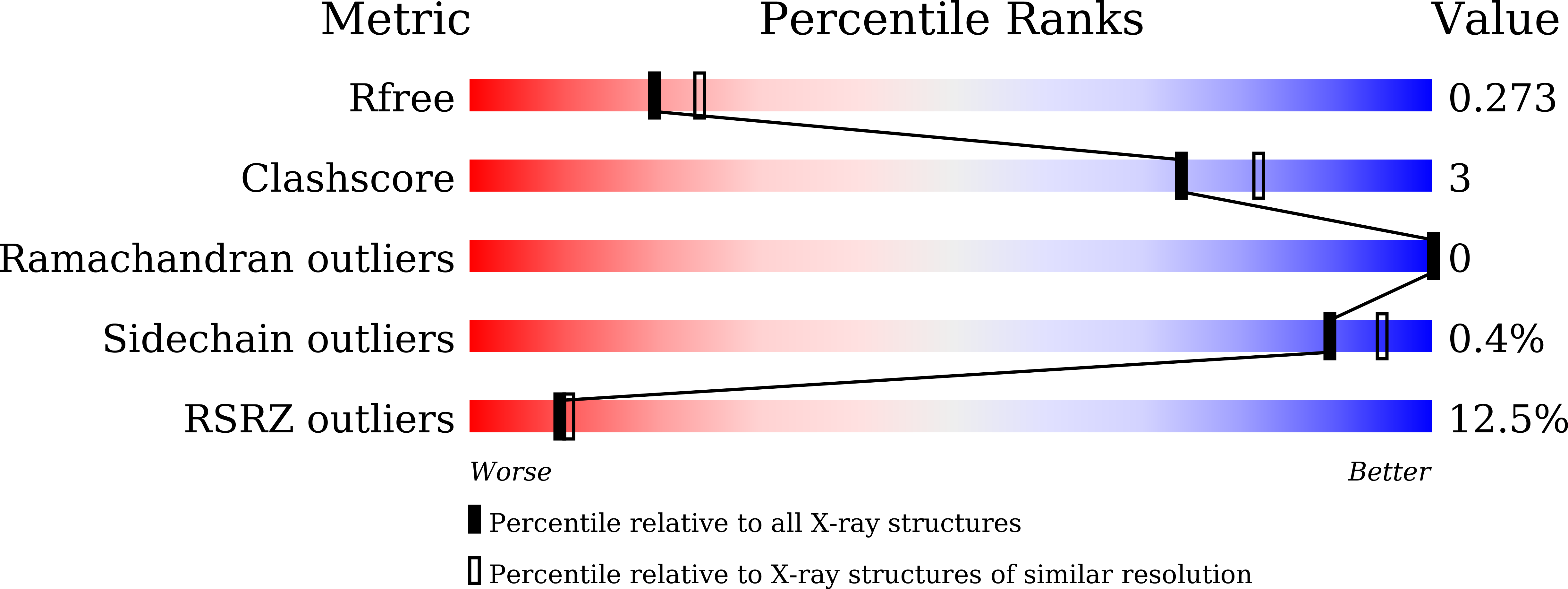
R-Value Free:
0.27
R-Value Work:
0.22
R-Value Observed:
0.22
Space Group:
I 1 2 1