Deposition Date
2015-10-14
Release Date
2015-10-28
Last Version Date
2024-11-06
Entry Detail
PDB ID:
5E8E
Keywords:
Title:
Crystal structure of thrombin bound to an exosite 1-specific IgA Fab
Biological Source:
Source Organism:
Homo sapiens (Taxon ID: 9606)
Method Details:
Experimental Method:
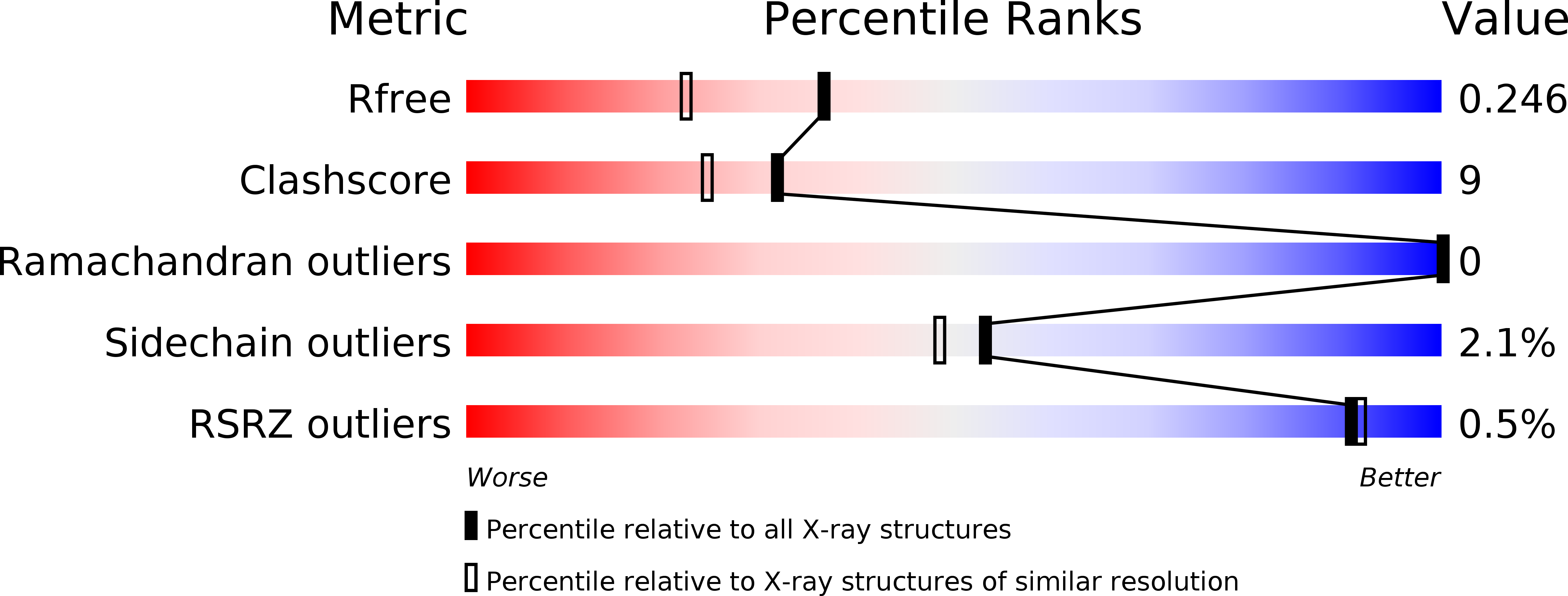
Resolution:
1.90 Å
R-Value Free:
0.24
R-Value Work:
0.20
R-Value Observed:
0.20
Space Group:
P 21 21 21